
The Anesthesia Gas Machine 2026
Michael P. Dosch PhD CRNA (ret), Darin Tharp CRNA MS
University of Detroit Mercy - Nurse Anesthesia
This site is https://healthprofessions.udmercy.edu/academics/na/agm/.
Revised Feb. 2026

The Anesthesia Gas Machine 2026
Michael P. Dosch PhD CRNA (ret), Darin Tharp CRNA MS
University of Detroit Mercy - Nurse Anesthesia
This site is https://healthprofessions.udmercy.edu/academics/na/agm/.
Revised Feb. 2026
What happens inside the workstation when oxygen pipeline pressure drops?
The fail safe device ensures that whenever oxygen pressure is reduced and until flow ceases, the set oxygen concentration shall not decrease at the common gas outlet (the point where gas prepared within the machine enters the breathing circuit). In addition, the loss of oxygen pressure results in high-priority audible and visible alarms.
Fail-safe systems don't prevent hypoxic mixtures in every possible circumstance. For example, as long as there is pressure in the oxygen line, nothing in the fail safe system prevents you from turning on a gas mixture of 100% nitrous oxide (however, this should be prevented by the hypoxic guard system, see below) or 100% of a third gas (e.g. helium if present)(which wouldn’t be prevented by the hypoxic guard, since the hypoxic guard only connects oxygen and nitrous oxide flowmeters).
Newer Drager machines (e.g. Fabius, Apollo) use a Sensitive Oxygen Ratio Controller (S-ORC). Its fail-safe component shuts off nitrous oxide if the oxygen flow is less than 200 mL/min, or if the oxygen fresh gas valve is closed. Audible and visible alarms sound if pipeline pressure (normally ~50 psi) is less than 20 + 4 psi. In case of complete oxygen pipeline failure, the machine will supply pipeline air so that oxygen 21% and agent can still be supplied to the patient.
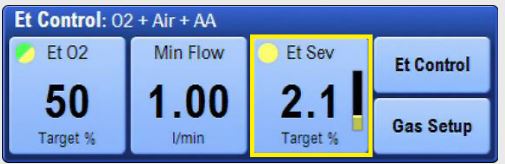
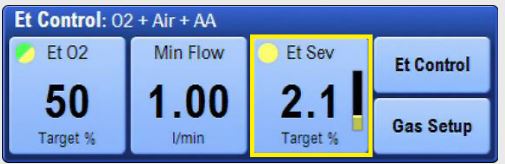
In the newest workstations (Aisys, A9, Perseus), the gas mixer prevents hypoxic breathing mixtures through electronic sensing and control of gas flows, pressures, and concentration. GE calls this End tidal Control (EtC); Mindray A9 calls it Automatic Controlled Anesthesia (ACA); Maquet calls it Automatic Gas Control with Active Hypoxic Guard.
|
EtC - End tidal Control. Click on the link to see the larger version. |
What should you do if you lose oxygen pipeline pressure?
Why? Something is wrong with the oxygen pipeline. What if the supply problem evolves into a crossover (non-oxygen gas in the oxygen pipeline)? Ifn that case, pipeline flow will continue (delivered at ~50 psi) rather than from your oxygen cylinder source (down-regulated to 45 psi). And unlike oxygen supply failure, which causes immediate, high priority audible and visible alarms, only the low FIO2 alarm will sound.
This is one reason you must calibrate the oxygen alarm each day by exposing it to room air for 1-2 minutes and ensuring it reads 21%. Even if you are only doing sedation; general anesthesia is always plan B. Starting a case with only a pulse oximeter but without an oxygen analyzer is like driving a car with a busted fuel gauge. You won't get an indication of a fuel problem until you are out of gas entirely. It's much smarter to hear an alarm at the beginning of an oxygen delivery problem (oxygen analyzer) than at the end (low saturation on the pulse oximeter), when hypoxemia is well established and the lung and your delivery system are completely devoid of oxygen.
So disconnect the pipeline connection at the wall if oxygen pipeline pressure is lost, or a crossover is occurring. It's easier to remember one strategy which works for both problems with the pipeline, than to remember that sometimes you must, and sometimes it is optional, to disconnect. And use that oxygen analyzer always!
Finally, ventilate by hand with the anesthesia breathing circuit, rather than with the mechanical ventilator (which uses cylinder oxygen for the driving gas if the pipeline is unavailable) or a bag-valve-mask (Ambu), because staying with the anesthesia breathing circuit means you can still deliver volatile agent.
Flowmeters differ in how they control and display gas flow.
| Control | Display | Example | |
|---|---|---|---|
| Glass |
Needle valve
|
Glass tube
|
Aestiva, Aespire |
| Hybrid |
Needle valve
|
Electronic
|
Apollo, Fabius |
| Gas Mixers |
Electronic
|
Electronic
|
Aisys, Avance, Perseus |
Or one can conceive of flowmeters by function: patient breathing gas, scavenger, common gas outlet, or auxiliary oxygen flow. Of course, we also measure flow (and volume, and composition) of inhaled and exhaled gases in the breathing circuit.
|
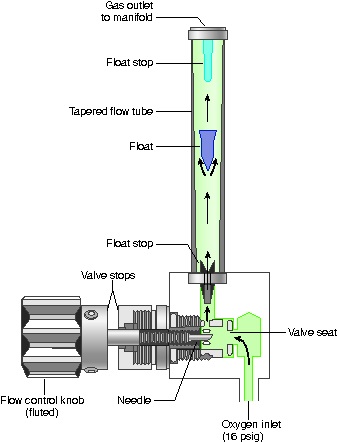
Glass flowmeter. Click on the link to see the larger version. |
In a traditional flowmeter, flow is mechanically controlled (needle valve) and displayed (glass tube with bobbin). A "Thorpe tube" is an older term for flowmeters. The components are- needle valve, indicator float, knobs, valve stops (in some). Flow increases when the knob is turned counterclockwise. At low flows, the annular-shaped orifice around the float is (relatively) tubular so (according to Poiseuille's Law) flow is governed by viscosity. At high flows (indicated on the wider top part of the float tube), the annular opening is more like an orifice, and density governs flows.
Flowmeters with mechanical needle valves and glass flowtubes are utilized in only a few current machines (Aespire, Aestiva).
|
|
Apollo flowmeters. Click on the link to see the larger version. |

|
Mindray A5 flowmeters (with common gas outlet flowmeter between the pressure gauges and below and to right of the oxygen flow knob). Click on the link to see the larger version. |
A hybrid flowmeter has characteristics that are transitional between glass flowmeters and fully electronic gas mixers. Flow is mechanically controlled (needle valve) and electronically displayed (bar graph on computer screen). Thus, hybrid flowmeters have no glass tubes or float bobbins. The flow rate is indicated with a bar graph on a monitor screen. There is a needle valve (so flow can be generated even without electric power) in the Apollo and Mindray A5. Flows are captured and displayed electronically. Thus, transitional (and electronic) flowmeters allow automated anesthesia record-keepers to chart fresh gas flows. To allow measurement of total fresh gas flow in the event of monitor screen failure or electrical power failure, these designs usually incorporate a common gas outlet flowmeter, which measures the total flow of all gases (oxygen plus carrier gas-either air or nitrous oxide).The common gas outlet flowmeter is visible in the first picture above, to the right of the Apollo needle valves.
|
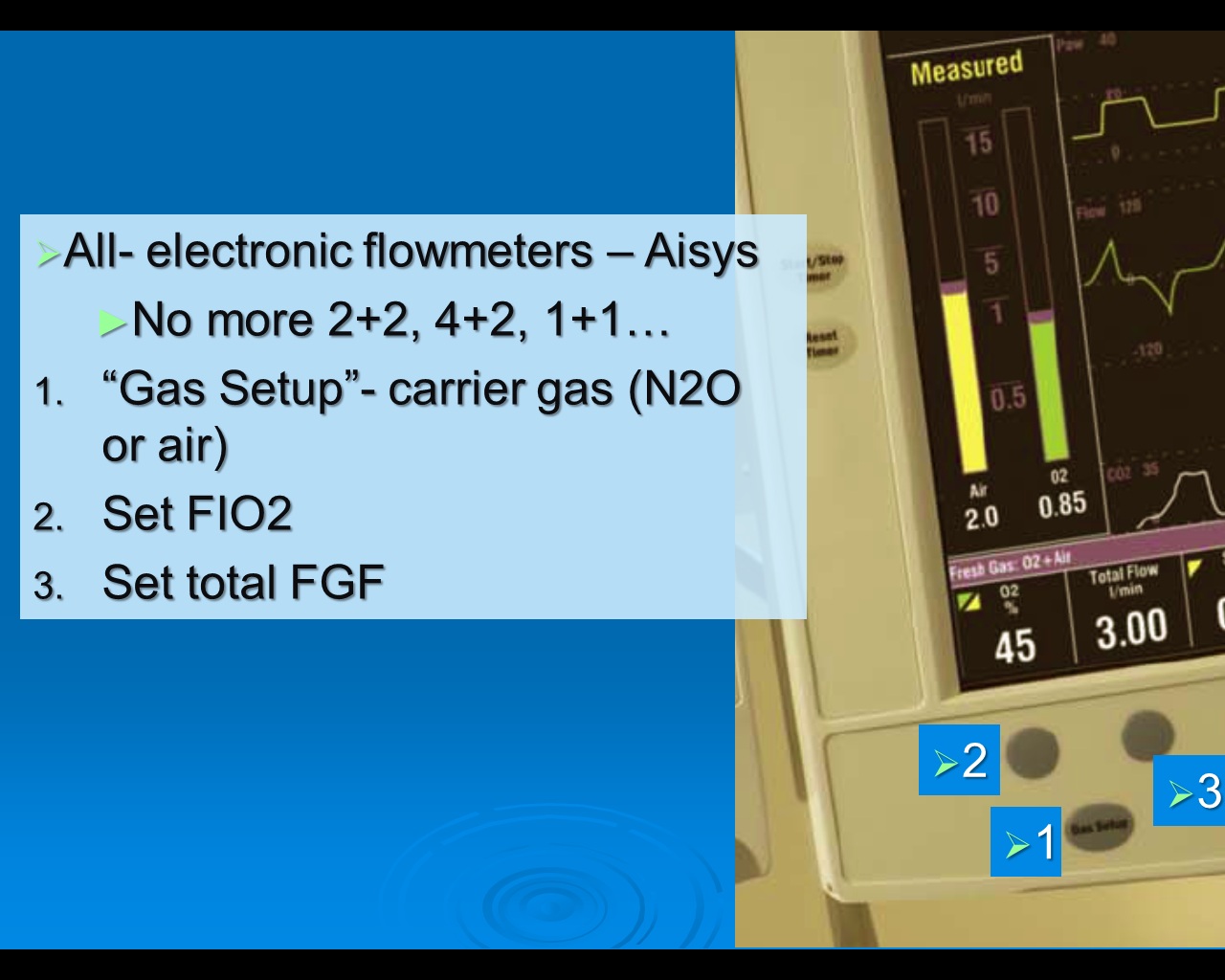
Aisys electronic flowmeters. Click on the link to see the larger version. |
Setting fresh gas flow on the Aisys, Avance, and Perseus is different. The gas mixer electronically controls flow of all gas and vapor to the patient, and these are displayed on a monitor screen. The user sets
It's an odd way to do it for anesthetists who are used to setting a process variable ("I'll use 2 L nitrous oxide + 2 L oxygen, which will give me 4 L/min FGF and therefore an FIO2 = 0.5") rather than setting the desired outcome (total FGF & FIO2 and letting the individual flows of air and nitrous oxide be determined by the machine ("I want a total flow of 4 L/min at an FIO2 of 0.5 in nitrous oxide").
|
EtC - End tidal Control. Click on the link to see the larger version. |
Electronic control of gas mix and fresh gas flow allows "Et Control" (in the GE Aisys CS2). Et control automatically adjusts fresh gas flow and dialed anesthetic agent (AA) to maintain expired oxygen (EtO2) and agent (EtAA) targets. The user sets the desired outcome (patient's end tidal oxygen & agent); the process of getting there (changing gas flows and agent concentration) is manipulated by the machine to produce the desired outcome quickly, and without further user intervention. This has the following advantages:
At the beginning of the case, it is entirely reasonable to activate Et Control immediately, to an EtAA of 0.5 MAC (to avoid post-induction hypotension). EtAA may then be increased in anticipation of incision. [3] At the end of the case, one can emerge the patient with EtC aid. There are two choices depending on the rapidity necessary. Select "Purge" and fresh gas flow is changed to 10 L/min with the vaporizer off, to flush agent and complete emergence as rapidly as possible. Selecting "Off" lets agent decrease gradually by stopping any further delivery of agent to the circuit (e.g. closes the vaporizer), while leaving FGF low. This results in a slower process whereby the patient "coasts" upwards towards readiness for extubation.
Besides the flowmeters which deliver gas to the breathing circuit, flowmeters are used in three other ways in the gas machine.

|
Location of scavenging flowmeter- Aisys. Click on the link to see the larger version. |
Choosing an appropriate fresh gas flow rate is covered below in the section "Delivery: Using breathing circuits and ventilators". Flowmeters on some machines have a minimum oxygen flow of 200-300 mL/min. Newer workstations have lower minimum oxygen flows (or no minimum oxygen flow at all). Supply pressure is pipeline oxygen at 50 psi.
Safety features - The oxygen flow control knob (if present) is touch-coded. If a gas has two glass flowtubes, they are connected in series. All gas flows first through fine, then through coarse flowtubes, controlled by a single flow-control knob. It is customary in the US for the oxygen flow tube to be on the right of the others, on the left in the UK. In either case, oxygen always enters the common manifold downstream of other gases.
Care of flowmeters with glass flowtubes includes ensuring that:
"Proportioning Systems" is the board exam terminology for the hypoxic guard system. These systems link nitrous oxide and oxygen flows (mechanically, pneumatically, or electronically) which is meant to prevent oxygen concentration less than 0.25 from being delivered to the breathing circuit when nitrous oxide is in use.
The potential flaws?

|
Maquet Automatic Gas Control. Click on the link to see the larger version. |
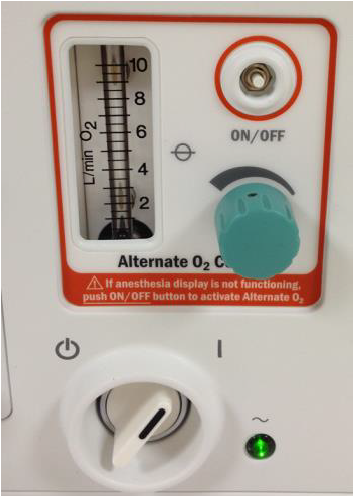
Newest workstations with electronic gas mixers (Aisys) supply a minimum delivered FIO2 of 25% with nitrous oxide, but will allow 21% if the carrier gas is air only. The hypoxic guard system includes desflurane on workstations with electronic gas mixers. These systems usually include an emergency backup knob and glass flowtube at the common gas outlet to indicate total FGF, because the gas mixer ceases to function if electric power fails. Automated gas control (as found on Maquet Flow-i workstation, or the Drager Zeus workstation) regulates inspired oxygen and expired agent concentration (as discussed above).
|
Aisys Alternate Emergency Oxygen. Click on the link to see the larger version. |
[1] Singaravelu S, Barclay P. Automated control of end-tidal inhalation anaesthetic concentration using the GE Aisys Carestation™. Br J Anaesth. 2013 Apr;110(4):561-6. doi: 10.1093/bja/aes464
[2] Tay S, Weinberg L, Peyton P, Story D, Briedis J. Financial and environmental costs of manual versus automated control of end-tidal gas concentrations. Anaesth Intensive Care. 2013 Jan;41(1):95-101. doi: 10.1177/0310057X1304100116
[3] Chang HK, Wen CH, Hung MH. Automated Volatile Anesthetics Delivery with End-tidal Control: Comment. Anesthesiology. 2026 Mar 1;144(3):735-736. doi: 10.1097/ALN.0000000000005852.
[4] Mudumbai SC, Fanning R, Howard SK, Davies MF, Gaba DM. Use of medical simulation to explore equipment failures and human-machine interactions in anesthesia machine pipeline supply crossover. Anesth Analg. 2010 May 1;110(5):1292-6. doi: 10.1213/ANE.0b013e3181d7e097
[5] AHRQ 2024 at https://psnet.ahrq.gov/web-mm/hypoxic-gas-supply-cross-connected-pipelines Accessed Feb 5, 2026.
[6] APSF Newsletter June 2019 at https://www.apsf.org/article/nitrogen-contamination-of-operating-room-oxygen-pipeline/ Accessed Feb 5, 2026.
[7] Pauling M, Ball CM. Delivery of Anoxic Gas Mixtures in Anaesthesia: Case Report and Review of the Struggle towards Safer Standards of Care. Anaesthesia and Intensive Care. 2017;45(1_suppl):21-28. doi:10.1177/0310057X170450S104.
[8] De Cooman S, Schollaert C, Hendrickx JF, Peyton PJ, Van Zundert T, De Wolf AM. Hypoxic guard systems do not prevent rapid hypoxic inspired mixture formation. J Clin Monit Comput. 2015 Aug;29(4):491-7. doi: 10.1007/s10877-014-9626-y. Note video content (scroll down).
[9] Eriksson S, Sixten B. More on the danger of inhaling air at reduced fresh gas flows: a self-experiment. J Clin Monit Comput. 2016 Apr;30(2):251-2. doi: 10.1007/s10877-015-9710-y.
[10] Carette R, De Wolf AM, Hendrickx JF. Automated gas control with the Maquet FLOW-i. J Clin Monit Comput. 2016 Jun;30(3):341-6. doi: 10.1007/s10877-015-9723-6.
[11] Ghijselings IE, De Cooman S, Carette R, Peyton PJ, De Wolf AM, Hendrickx JF. Performance of an active inspired hypoxic guard. J Clin Monit Comput. 2016 Feb;30(1):63-8. doi: 10.1007/s10877-015-9684-9.