
The Anesthesia Gas Machine
Michael P. Dosch CRNA PhD
University of Detroit Mercy - Nurse Anesthesia
This site is https://healthprofessions.udmercy.edu/academics/na/agm/index.htm.

The Anesthesia Gas Machine
Michael P. Dosch CRNA PhD
University of Detroit Mercy - Nurse Anesthesia
This site is https://healthprofessions.udmercy.edu/academics/na/agm/index.htm.
Revised May 2025
 "Hanging" bellows. Click on the thumbnail, or on the underlined text, to see the larger version.
"Hanging" bellows. Click on the thumbnail, or on the underlined text, to see the larger version.
To remember the classification: "ascend" and "descend" have "e" in them - so look at them during expiration. Ascending bellows ("standing") ascend during expiration (modern type - preferred) and descending bellows ("hanging") descend during expiration. Ventilator relief valve gives 2 - 3 cm water pressure positive end-expiratory pressure (PEEP) (true for all mechanical ventilators with standing bellows). The ventilator relief valve (spill valve) allows scavenging ONLY during the expiratory phase.
"Hanging" bellows on the Anestar. Click on the thumbnail, or on the underlined text, to see the larger version.
The hanging design is chosen by a (very) few manufacturers. Newer hanging bellows housings, unlike older designs, lack an internal weight, and sense when the bellows do not return to the full "down" position. These factors, plus integration of disconnect alarms based on chemical (capnograph), and mechanical (pressure, volume, and flow sensors) apnea detection, make hanging bellows designs safe. However, placement of the hanging bellows below the writing surface can make visual detection of disconnects difficult. Also it is less easy to determine if the patient is breathing spontaneously in addition to the rate set on the mechanical ventilator. The user must rely more on the pressure and capnography waveforms as opposed to the bellows. Water may gather in the descending bellows (lessening tidal volume and creating an infection risk) but this tendency may be counteracted by heating the absorber head.
Besides increased accuracy in volume control ventilation (VCV) (due to compliance and leak compensation- see below on this page), the biggest improvement in current ventilators is their flexibility in modes of ventilation. Offering pressure controlled ventilation (PCV) allows more efficient and safe ventilation of many patients. The improvement in ventilator sensors and electronic controls means that switching of circuits (for example, to a non-rebreather for small children) is not as necessary. This is safer because potential misconnections are avoided, and quicker besides. The latest direction the manufacturers have taken is offering modes (such as pressure support) that will support or assist spontaneous ventilation, seen in anesthesia with much greater frequency due to the advent of the laryngeal mask airway and more brief ambulatory procedures.
Terminology for modes and controls is not standardized, and can be confusing. The table below gives Dräger and GE terminology for ventilator mode classification.
Sources - see footnote 2.
| Manufacturer | Model | Ventilator type | Modes |
|---|---|---|---|
| Dräger Medical | Perseus A500 | Turbine | Manual/spontaneous, PC-CMV, PC-BIPAP, VC-CMV, VC-CMV/AF, VC-SIMV/AF. Optional: SPN-CPAP/PS, PC-BIPAP/PS, VC-SIMV/AF/PS, PC-APRV. |
| Dräger Medical | Apollo | Piston | Manual/spontaneous, VC-CMV, PC-CMV. Optional: PS, VC-CMV/AF. |
| GE Healthcare | Aisys-CS2 | Bellows | Manual/spontaneous, VC-CMV. Optional: PC-CMV, PCV-VG, SIMV (with VC-CMV, PC-CMV, or PC-VG), SPN-CPAP/PS. |
Sources- see footnote 3.
Waves- VC-CMV. Click on the thumbnail, or on the underlined text, to see the larger version.
All ventilators offer volume controlled ventilation (VCV is the GE terminology). In this mode, the set volume is delivered at a constant flow. The peak inspiratory pressure is allowed to vary, and it does, according to the patient's compliance and airway resistance. Volume is adjusted to avoid atelectasis, and rate is adjusted for reasonable end-tidal carbon dioxide while monitoring the peak inspiratory pressure.
The values controlled and kept at the set target value are the tidal volume (VT) and respiratory rate (RR, breaths/min, f). This results in the minute volume (MV = f x VT). The duration of the inspiratory phase is defined by the inspiration time (Ti). If the inspiratory flow is so high that the set breathing volume is reached before the set inspiratory time (Ti) has passed, there will be a pause in inspiration.
VC-CMV, once universal, is much less frequently used at present, in view of better alternatives such as PC-SIMV-VG.
Waves- VC-SIMV. Click on the thumbnail, or on the underlined text, to see the larger version.
VC-SIMV detects spontaneous breaths (if any) and delivers volume-controlled breaths in synch with the patient's inspiratory efforts. This helps maintain minute ventilation, while avoiding breath-stacking or bucking. If too many (or too few) synchronized breaths are delivered, adjust trigger window and sensitivity.
Patients may breathe at will between ventilator breaths. The AIsys/Avance ventilators in VCV mode support any "in-between" spontaneous breaths with pressure support ventilation (PSV), resulting in a mode GE calls SIMV-PS.
Waves- PC-CMV. Click on the thumbnail, or on the underlined text, to see the larger version.
PC-CMV controls inspiratory pressure (Pinsp), PEEP, and f (breaths/min). The pressures are also maintained in case of leakage. Tidal volume (and MV) vary with changes in patient effort, compliance and airway resistance. The flow generated varies. Flow is high at first to produce the set Pinsp early in inspiration, and it is less later in inspiration to maintain the set pressure through the inspiratory time (Ti). This is known as a decelerating flow (or ramp) pattern, which is thought to be beneficial in gas exchange and ventilation perfusion matching (this is controversial- see footnote 4).
Target pressure is adjusted to produce a reasonable VT (reasonable to avoid the extremes of atelectasis and volutrauma). Rate is adjusted to a reasonable end-tidal carbon dioxide. The result (in many instances where peak inspiratory pressure [PIP] had been high when employing VCV [e.g. laparoscopy]) is often that PCV delivers increased tidal volume at a lower PIP. How is this possible? The answer is that the flow of gas is greater early in inspiration (see waveforms above). Overall this may result in greater delivered volume with the same (or lower) pressure. "Slope" adjusts how quickly the higher pressure level is reached. The Pinsp is maintained for the duration Ti (this time control is not used in PC-PSV).
Pressure controlled modes, especially those which incorporate SIMV, PSV, and Volume guarantee, are often a default mode on new workstations.
If there is a danger of high PIP, use PC-CMV to limit pressure within the airway and lungs.
If compliance is low, use PC-CMV to obtain a higher tidal volume.
PC-CMV is also used to compensate for leaks
PC-CMV-VG. Click on the thumbnail, or on the underlined text, to see the larger version.
PC-CMV, but a tidal volume target is also set. The ventilator then dynamically adjusts the Pinsp (while staying within the set maximum pressure [Pmax]) to achieve the desired VT breath-by-breath. Advantages include control of PIP (through the basic pressure-controlled mode) and control of arterial CO2 (through guarantee of VT and thus minute ventilation). Volume guarantee may be used with pressure-controlled modes such as PC-SIMV, PC-CMV and PC-PSV. Volume guarantee ensures that for all mandatory breaths the set tidal volume (VT) is applied with the minimum pressure necessary. If the Resistance (R) or Compliance (C) changes, the pressure adapts gradually (over 4 or so breaths) in order to return delivered VT to the set target VT.
Waves- PC-SIMV. Click on the thumbnail, or on the underlined text, to see the larger version.
SIMV can be pressure controlled, resulting in a mode called SIMV-PC. You will notice from examining the waves, that PC-SIMV with PEEP and PSV is very like PC-BiPAP.
Waves- PC-BiPAP. Click on the thumbnail, or on the underlined text, to see the larger version.
The patient can breathe spontaneously at any time. Mandatory breaths are synchronized with the breathing attempts of the patient. If no spontaneous breathing attempt is detected during the inspiratory trigger window, the machine-triggered mandatory breath is applied. The VT results from the pressure difference between PEEP and Pinsp, the lung mechanics and the breathing effort of the patient. If the Resistance (R) or Compliance (C) of the lung changes, VT and MV also vary. During spontaneous breathing at PEEP level, the patient can be supported using PS. If lacking this mode, it can be simulated with PC-PSV mode with appropriate values for Pinsp and PEEP.
With the advent of the LMA, spontaneous (unassisted) breathing is much more common during general anesthesia. But it is difficult to maintain a light enough plane of anesthesia to permit spontaneous ventilation, while retaining sufficient depth for surgery to proceed. Too deep, and respiratory acidosis will occur; too light, and bucking and awareness are risks. Ventilation modes which support the spontaneously breathing patient are useful to provide normocapnia without bucking. Many ventilators currently incorporate pressure support ventilation (PSV). Continuous positive airway pressure (CPAP), and airway pressure release ventilation (APRV) have now been implemented on various models of anesthesia workstations.
During the spontaneous ventilation modes, the patient carries out the majority of the breathing effort. The pressure level PEEP (CPAP) at which spontaneous breathing takes place, can be adjusted. In all spontaneous ventilation modes, the spontaneous breaths can be supported mechanically. To suit the respective lung mechanics, the speed of the pressure increase for PS (Pressure Support) and VS (Volume Support) can be defined using the slope or flow adjustment. Both adjustments, slope and flow, thus define the duration of the pressure increase from the lower to the higher pressure level. With the slope adjustment the time is set in seconds, with the flow adjustment the gas flow is set in liters per minute. This setting directly affects the flow and thus the supplied tidal volume (VT).
Waves- PSV. Click on the thumbnail, or on the underlined text, to see the larger version.
In PSV, every detected inspiration attempt at PEEP level triggers a patient-triggered, flow-cycled, pressure-supported mandatory breath. The point of time, the number and the duration of the pressure-supported breaths are determined by the patient. If the lung mechanics of the patient change, the VT varies. Settings for PSV are simple- just Psupp (the inspiratory pressure support level- try 10 to 12 cm H2O to start) and PEEP (the "expiratory support level," if that makes sense). Psupp should be adjusted to VT of 5-7 mL/kg ideal body weight. Note that PSV requires a spontaneously breathing patient as there is no mandatory minimum respiratory rate. PEEP is ordinarily used with PSV to help recruit alveoli.
PSV senses patient inspiratory effort (volume or flow) and delivers pressure support while it is present. This tends to result in larger VT than the patient would produce on their own. PSV is useful to support minute ventilation and control arterial carbon dioxide for spontaneously-breathing patients during maintenance or emergence.
In the Aisys, PSV-Pro ("protect") is found. If no breaths are detected during an adjustable apnea delay period (10-30 sec), the ventilator switches to the backup mode (PCV, at backup settings of Pinsp and RR). If resumption of spontaneous breaths occurs later, the ventilator will return to PSV-Pro mode.
SPN-CPAP with ARM (alveolar recruitment maneuver). Click on the thumbnail, or on the underlined text, to see the larger version.
In SPN-CPAP, the patient breathes at the PEEP level (expiratory support) with Psupp = 0 (no inspiratory support). Compared to the atmospheric pressure, the airway pressure is increased during the complete breathing cycle. If the patient is too weak to manage breathing effort completely independently, pressure support (PSV) is an option.
Waves- PC-APRV. Click on the thumbnail, or on the underlined text, to see the larger version.
In PC-APRV, the patient’s spontaneous breathing takes place at the upper pressure level "Phigh". Phigh is maintained for the duration of Thigh (time at high pressure). To execute an active expiration and support CO2 elimination, the pressure is reduced (to Plow) for the brief period (Tlow). The alternation between the two pressure levels is machine-triggered and time cycled. The breathing volume (VT) expired during the relief times (at Plow), results from the pressure difference between Plow and Phigh and the lung mechanics. If the Resistance or Compliance of the lung changes, the VT and thus the minute volume MV also vary.
Ventilator-associated lung injury is caused by overinflation of some lung areas (volutrauma), excess PIP (barotrauma), underinflation and derecruitment of other areas (atelectrauma), and an increase in inflammatory mediators resulting from alveolar wall stress (biotrauma). See footnote 5. There is also a nice section of the Draeger web site on protective ventilation.
While no one "recipe" works for all patients or all situations, certain themes have emerged from the research which are probably useful for most patients:
All current gas machines have VPO (volume, pressure, oxygen) monitoring built in the breathing circuit. Most have agent monitoring as well. Some have spirometry and capnography.
Turbines have been used in the ICU for years, but until recently were not found on anesthesia ventilators. Turbines are an efficient means of generating inspiratory flow quickly, thus they are well-suited to deliver patient-triggered breaths. The TurboVent 2 on Perseus A500 (Dräger) is a compressor/blower which generates the pressure required for ventilation. During inspiration, TurboVent 2 rapidly (in milliseconds) increases the rotation speed to create the set inspiratory pressure (imagine a super powerful hair dryer). It spins at a low rate during expiration also. This maintains PEEP, and also a flow of 0.6 L/m though the breathing circuit, in order to improve mixing of gases in the circuit, and lessen the work of breathing of any small spontaneous breaths.
The maximum inspiratory flow is 180 L/m (higher than any current anesthesia ventilator). Operation is controlled electronically, based on data from the pressure and flow sensors contained in the breathing system. The ventilation pressure and flow during inspiration and expiration are attained by means of the turbine and the Pmax/PEEP flow valve in the breathing system.
Perseus breathing circuit. Click on the thumbnail, or on the underlined text, to see the larger version.
The turbine draws inspiratory volume from the manual breathing bag as well as from fresh gas flow. The manual breathing bag moves during mechanical ventilation, but in a direction opposite to Apollo. In the Perseus, the manual breathing bag empties during inspiration (like a bellows), and fills during expiration. Thus, the circuit differs from Apollo in two aspects: 1) it lacks a decoupling valve, and 2) the Pmax/PEEPvalve was moved from proximal (upstream) of the expiratory unidirectional valve, to downstream from it.
Consequences from the turbine technology:
See footnote 6
Fabius piston (middle left in figure). Click on the thumbnail, or on the underlined text, to see the larger version.
Piston ventilators use an electric motor to drive a piston, which compresses gas in the breathing circuit, creating the motive force for inspiration to occur. Thus a piston ventilator uses no driving gas, and may be used without depleting the oxygen cylinder in case of oxygen pipeline failure.
Compliance losses are significantly decreased by omitting the compressible bellows. If the corrugated limbs are expanded before the morning electronic self-test of compliance and leaks, the compliance losses out to the Y-piece are known. Thereafter, all that is required is a pressure sensor anywhere in the breathing circuit to deliver accurate VT.
Apollo interface. Click on the thumbnail, or on the underlined text, to see the larger version.
In the Apollo, the bellows operation is not visible. The anesthetist relies on flow, pressure, and capnography waveforms (and the movement of the breathing bag during mechanical ventilation as a result of fresh-gas decoupling [see section on fresh gas decoupling below on this page]) to guard against disconnects or other problems.
 Apollo waveforms - ETCO2, Flow-time, Pressure. Click on the thumbnail, or on the underlined text, to see the larger version.
Apollo waveforms - ETCO2, Flow-time, Pressure. Click on the thumbnail, or on the underlined text, to see the larger version.
Piston ventilator window Fabius GS. Click on the thumbnail, or on the underlined text, to see the larger version (35 KB).
The Fabius GS has a piston ventilator similar to the Apollo, but the bellows travel vertically, and its movement is continuously visible through a window to the left of the flowmeter bank.
Piston ventilators have positive and negative pressure relief valves built in. If the pressure within the piston reaches 75 + 5 cm H2O, the positive pressure relief valve opens. If the pressure within the piston declines to -8 cm H2O, the negative pressure relief valve opens, and room air is drawn into the piston, protecting the patient from NEEP (negative end-expiratory pressure).
There are several advantages to a piston ventilator system (Apollo & Fabius GS):
The disadvantages of the piston design include:
The appearance of pressure control ventilation is a major advantage, allowing patients to be ventilated efficiently who were very difficult with volume control mode, such as patients with ARDS or morbid obesity. PCV also allows safe ventilation when excessive pressure must be strictly avoided; such as neonates and infants, and emphysematous patients. The appearance of modes which are capable of supporting the patient with spontaneous respirations (like PSV, SIMV, CPAP, and Volume Guarantee) extends our capabilities further.
(This section only refers to increasing VT accuracy during volume control ventilation, which is hardly ever used at present.)
Factors contributing to a discrepancy between set and delivered tidal volumes in VCV are especially acute in pediatrics and include
Because of the greatly increased accuracy in tidal volume delivery achieved through compliance and leak testing and compensation, modern ventilators have an unprecedented tidal volume range. They are able to ventilate smaller patients in VC-CMV mode much more accurately than any previous anesthesia ventilator could (see footnote 7). Anything that lessens the need for non-rebreathing (Mapleson & Bain) circuits, which is safer, since anesthetists will no longer have to disassemble and reconfigure to a non-rebreathing circuit for a child in the middle of several adult cases. PCV is of course much more commonly used in children and adults, as stated, which also plays a role in the decreased need for non-rebreathing circuits. Regardless of mode, it is wise to substitute a pediatric circuit for tidal volumes less than 200 mL, in order to lessen compliance losses to the corrugated hoses (see footnote 8).
|
Ventilator
|
Range of VT (mL) in VC-CMV
|
| Fabius GS | 20-1400 |
| Apollo | 20-1400 |
| Aestiva | 20-1500 |
| Perseus | 20-2000 |
| Aisys | 20-1500 |
An electronic leak and compliance test must be repeated every time the circuit type is changed (e.g. adult circle to pediatric circle, or adult to long circuit). This test is part of the electronic self-test portion of the morning checklist.
The placement of the sensor used to compensate tidal volumes for compliance losses and leaks has some interesting consequences. All flow and volume sensors are somewhat sensitive to moisture accumulation, which is more likely due to rebreathing as fresh gas flows decrease. The Aestiva flow sensors are placed between the disposable corrugated breathing circuit limbs and the absorber head. Here they are able to compensate tidal volumes for fresh gas flow, compliance losses and leaks internal to the machine and absorber head- but not in the breathing hoses. Apollo, Perseus, and Aisys test compliance and leaks of all components to the Y-piece via pressure transducer and flow sensors within the internal circuitry near the bellows. Here the sensors are somewhat protected from moisture. Aisys relies on an optional (but recommended) condenser to keep the breathing circuit dry and protect the flow sensors; Perseus uses a heated absorber head.
Modern ventilators compensate delivered tidal volume for changes in fresh gas flow (FGF). In older ventilators, which are not fresh gas decoupled, the delivered tidal volume is the sum of the volume delivered from the ventilator bellows, and the fresh gas flow delivered during the inspiratory phase of each breath. Thus, delivered tidal volume may change as FGF is changed.
| Example |
|---|
For example, consider a patient with a FGF of 4 L/min, a respiratory rate of 10, inspiratory:expiratory (I:E) ratio of 1:2, and a tidal volume of 700 mL. During each minute, the ventilator spends 20 seconds in inspiratory time and 40 seconds in expiratory time (1:2 ratio). During this 20 seconds, the fresh gas flow is 1,320 mL (4000 mL/min FGF times 20/60 sec). Each of the 10 breaths of 700 mL is augmented by 132 mL of fresh gas flowing while the breath is being delivered, so the total delivered tidal volume is 832 mL/breath. This 19% increase is reasonably unimportant since we target settings to etCO2. But what happens if we decrease the fresh gas flow? Assume the same parameters, but a FGF of 1,000 mL/min. During each minute, the ventilator spends 20 seconds in inspiratory time and 40 seconds in expiratory time (1:2 ratio). During this 20 seconds, the fresh gas flow is 330 mL (1000 mL/min FGF times 20/60 sec). Each of the 10 breaths of 700 mL is augmented by 33 mL of fresh gas flowing while the breath is being delivered, so the total delivered tidal volume is 733 mL/breath. This means that changing FGF from 4,000 mL/min to 1,000 mL/min, without changing ventilator settings, has resulted in a 14% decrease in delivered tidal volume (832 to 733 mL). It would not be surprising if the end tidal carbon dioxide rose as a result. The situation is more acute with an older anesthesia ventilator in children. Assume a 20 kg patient with a FGF of 4 L/min, a respiratory rate of 20, inspiratory:expiratory ratio of 1:2, and a tidal volume of 200 mL. During each minute, the ventilator spends 20 seconds in inspiratory time and 40 seconds in expiratory time (1:2 ratio). During this 20 seconds, the fresh gas flow is 1,320 mL (4000 mL/min FGF times 1/3). Each of the 20 breaths of 200 mL is augmented by 66 mL of fresh gas flowing while the breath is being delivered, so the total delivered tidal volume is 266 mL/breath. This is a 33% increase above what is set on the ventilator. We now decrease the FGF from 4 to 1 L/min for the same 20 kg child, (RR 20, I:E ratio of 1:2, and VT 200 mL). During each minute, the ventilator spends 20 seconds in inspiratory time and 40 seconds in expiratory time (1:2 ratio). During this 20 seconds, the fresh gas flow is 333 mL (1000 mL/min FGF times 1/3). Each of the 20 breaths of 200 mL is augmented by 16.5 mL of fresh gas flowing while the breath is being delivered, so the total delivered tidal volume is 216 mL/breath. This is a 23% decrease in VT (266 to 216 mL/breath) caused solely by changing FGF, and without altering vent settings. |
Fabius GS ventilator schematic. Click on the thumbnail, or on the underlined text, to see the larger version (39 KB).
There are two approaches to dealing with the problem. The Dräger Apollo and Fabius GS use fresh gas decoupling. Fresh gas is diverted by a decoupling valve to the manual breathing bag during inspiration, and is thus not added to the delivered tidal volume. Thus, fresh gas decoupling helps ensure that the set and delivered tidal volumes are equal.
The action of the piston closes a one-way (decoupling) valve, diverting FGF to the manual breathing bag during the inspiratory cycle. The visual appearance is unusual:
With fresh gas decoupling, if there is a disconnect, the manual breathing bag rapidly deflates, since piston retraction draws gas from it.
The second approach is fresh gas compensation, which is utilized in the Aisys, Aestiva, Avance, and Aespire. The volume and flow sensors provide feedback which allows the ventilator to adjust the delivered tidal volume so that it matches the set tidal volume, in spite of changes in the total fresh gas flow.
Perseus breathing circuit. Click on the thumbnail, or on the underlined text, to see the larger version.
A similar approach is taken in the Dräger Perseus. The breathing circuit is like Apollo, but has no fresh gas decoupling valve. The placement of the fresh gas flow (FGF) inlet between turbine and inspiratory unidirectional valve means that FGF is not diverted to the reservoir bag during inspiration (as in Apollo or Fabius), but is added to VT during inspiration. Data from flow and pressure sensors is used to control turbine speed. The Pmax/PEEP valve, which stops inspiration when the desired VT and inspiratory time (Ti) are achieved. In Perseus (opposite to Appollo or Fabius), the bag behaves like a standing bellows- deflating during inspiration and inflating during expiration.
Low fresh gas flow is desirable to reduce pollution and cost of volatile agents and nitrous oxide, preserve tracheal heat and moisture, prevent soda lime granules from drying, and preserve patient body temperature. Factors which enhance the safety and efficiency of low flows in modern ventilators include:
 |
Apollo. Click on the thumbnail, or on the underlined text, to see the larger version (96 KB).
|
 |
Apollo controls. Click on the thumbnail, or on the underlined text, to see the larger version (105 KB). |
The Apollo is a modern piston ventilator with spirometry monitoring. The piston ventilator is electrically driven and electronically controlled, fresh gas decoupled. Ventilation modes Manual, spontaneous, VCV, PCV, SIMV-Vol, SIMV-PC, PSV. Optional/Synchronization: Pressure Support (PS).
 |
Perseus. Click on the thumbnail, or on the underlined text, to see the larger version.
|
 |
Perseus controls. Click on the thumbnail, or on the underlined text, to see the larger version. |
Possible control settings for Perseus in PC-SIMV mode. Click on the thumbnail, or on the underlined text, to see the larger version.
The Perseus is a modern turbine ventilator. The turbine ventilator is electrically driven and electronically controlled. It works without compressed gas. Ventilation modes are extensive, including the first availability of APRV and CPAP on an anesthesia ventilator. Much like an ICU ventilator in the sophistication of its controls: ventilation can be optimized for a very wide range of patients and situations. However, it does place a learning burden on anesthetists, who must learn the new controls and their interactions.
| Fabius GS ventilator controls and piston window (left of flowmeters). Click on the thumbnail, or on the underlined text, to see the larger version (36 KB). | |
|
Fabius GS Ventilator controls. Click on the thumbnail, or on the underlined text, to see the larger version (57 KB).
|
The Fabius GS ventilator is an electronically controlled, electrically driven piston ventilator. It consumes no drive gas. The piston is continuously visible. Operating parameters include
 |
Aisys. Click on the thumbnail, or on the underlined text, to see the larger version.
|
|
Aisys controls. Click on the thumbnail, or on the underlined text, to see the larger version.
|
|
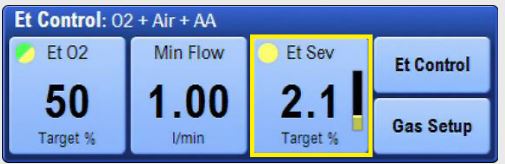 |
End tidal Control. Click on the thumbnail, or on the underlined text, to see the larger version.
|
The Aisys has a dual circuit, ascending bellows 7900 ventilator. Modes include VCV, PCV, PC-VG, SIMV-Vol, SIMV-Press, and PSV-Pro. Maximum flow is 120 L/min. Maximum pressure is 60 cm H2O. PEEP 0-30 cm H2O. Inspiratory/expiratory ratio can be selected from 2:1 to 1:8. The vent features tidal volume compensation, one switch activation from manual to mechanical ventilation,two key presses to total standby (end case), and a cardiac bypass case mode.
The Advanced Breathing System (ABS™) has a minimal number of parts and tube connections, which greatly reduces the potential for leaks and misconnects. It is easy to disassemble (no tools), fully autoclavable, and latex-free (as are most modern anesthesia machines). The Aisys CS2 features End Tidal Control, by which the users sets targets for expired agent, oxygen,and minimum fresh gas flows, and the machine manipulates FGF and agent concentration to achieve and maintain these targets more quickly and with less control interactions with the operator.
|
Avance. Click on the thumbnail, or on the underlined text, to see the larger version (151 KB).
|
 |
Aespire. Click on the thumbnail, or on the underlined text, to see the larger version (414 KB).
|
| 7100 controls . Click on the thumbnail, or on the underlined text, to see the larger version (43 KB). |
Aespire (and Aestiva) share the current GE 7100 ventilator. Aespire shares the Advanced Breathing System used by Aisys and Avance. The 7100 ventilator features VCV, PCV, and electronic PEEP. VT range is 45-1500 mL. Maximum inspired pressure is 50 cm water.
| Aestiva/5 with 7100 ventilator. Click on the thumbnail, or on the underlined text, to see the larger version (31 KB). |
|
Paragon breathing circuit. Click on the thumbnail, or on the underlined text, to see the larger version (157 KB).
|
|
|
AV-S ventilator. Click on the thumbnail, or on the underlined text, to see the larger version (48 KB).
|
The breathing circuit is latex free, like most modern machines. Absorbent capacity is 1.3 kg of loose or pre-packed absorbent. The standing bellows may be driven by oxygen or air.
The AV-S ventilator on the Paragon Platinum SC430 offers integrated FGF compensation, VPO (volume, pressure, oxygen) and spirometry monitoring, and automated compliance and leak testing. VCV (20-1600 mL/breath), PCV (to 70 cm H2O), and PSV modes are available with integrated electronic PEEP. Insp/Exp ratio is selectable from 1:0.3 to 1:8. Pmax 80 cm H2O.
| Anestar. Click on the thumbnail, or on the underlined text, to see the larger version (367 KB).
|
The Anestar ventilator is a hanging bellows, gas-driven, electronically controlled ventilator. It offers VCV, PCV, and PSV modes. VT is 10-9999 mL. Insp/Exp ratio is 3:1 to 1:5. The breathing circuit is warmed and VT compensation is achieved through fresh-gas decoupling. Flow sensors are hot-wire anemometers (like most Draeger machines). The internal volume of the breathing system is 2.5 L (of which 1.4 L is absorbent).
How do you determine that a machine needs replacement? See footnote 9).
 |
Photograph of the ADU ventilator controls. The left arrow shows the Bag/Auto and APL valve location. The right arrow shows the location of the thumbwheel and buttons by which ventilator settings are changed. Click on the thumbnail, or on the underlined text, to see the larger version (92 KB).
|
|
Photograph of the D-Lite sensor. Click on the thumbnail, or on the underlined text, to see the larger version (46 KB).
|
The ADU ventilator has a suite of useful and unique features, many of which it shares with other modern anesthesia ventilators. Single switch activation (setting the Bag/Vent switch to "Auto") is all that is needed to start mechanical ventilation (all new ventilators are activated in this way). Entering the patient’s weight will suggest appropriate ventilator settings. Delivered VT is adjusted to compensate for changes in fresh gas flow, and total (absorber head and corrugated limbs) breathing circuit compliance losses through the D-Lite sensor at the elbow.
The ventilator can utilize either oxygen or air as a driving gas, and will switch automatically if oxygen pipeline pressure is lost. Volume-control, pressure control, synchronized intermittent mandatory ventilation (SIMV-Vol),and PSV modes are offered, along with integrated electronic PEEP. Overpressure release valve at 80 cm water means that patients requiring higher peak inspiratory pressure cannot be ventilated in volume control mode (but they may be ventilated successfully in pressure control mode).
The pressure control mode should be very useful to increase delivered tidal volume when lung compliance is low (laparoscopic procedures, obesity, pregnancy) or when high peak inspiratory pressures must be avoided (pediatric patients, laryngeal mask ventilation, emphysema). Flow-volume (resistance) or pressure-volume (compliance) loops may be displayed breath-by-breath.
 |
NM 6000 piston bellows and ventilator controls (front panel). Click on the thumbnail, or on the underlined text, to see the larger version (44 KB).
|
|
Divan Controls (front panel). Click on the thumbnail, or on the underlined text, to see the larger version (78 KB).
|
The Dräger Divan ventilator is a modern ventilator, offering features such as: pressure control mode, SIMV, correction for compliance losses, and integrated electronic PEEP. Unlike the ADU, newer Dräger absorber heads warm the gases in the breathing circuit. Also unique is that fresh gas flow does not add to delivered tidal volume ("fresh gas decoupling"- see New features above on this page). The Divan is limited to a pressure of 70 cm water- so it cannot ventilate patients in VCV mode beyond this pressure (although, again, it is possible and even perhaps preferable to ventilate the ARDS patient with pressure control mode). It is installed on the Narkomed 6000/6400.
Unlike most other anesthesia ventilators, there are no visible bellows on the NM6000 Divan ventilator. It is unique among current models in having a horizontal piston which is hidden within the writing surface of the gas machine. To provide a visible indication of lung inflation, fresh gas is diverted to the manual breathing bag, which inflates during mechanical ventilator inspiration, and deflates during expiration. A disconnect will cause the manual breathing bag to gradually lose volume (in addition to activating other apnea alarms). A pressure transducer within the ventilator measures compliance losses and leaks in the total breathing circuit (absorber head and corrugated limbs).
The Fabius GS has a piston ventilator as well, but the piston is mounted vertically to the left of the flowmeters and is visible through a window.
 AV2 controls. Click on the thumbnail, or on the underlined text, to see the larger version (46 KB).
AV2 controls. Click on the thumbnail, or on the underlined text, to see the larger version (46 KB).
Classification: pneumatically and electrically powered, double circuit, pneumatically driven, ascending bellows, time cycled, electronically controlled, VT-preset vent. Incorporates Pressure Limit Controller (PLC) which allows maximum peak inspiratory pressure (PIP) adjustment from 10-110 cm water. Inspiratory flow control must be set properly (like the Ohmeda 7800), so that driving gas flow does not create an inspiratory pause. Standard on Narkomed 2A, 2B, 2C, 3, 4, and Narkomed (not Fabius) GS.
 Ohmeda 7000 controls. Click on the thumbnail, or on the underlined text, to see the larger version (43 KB).
Ohmeda 7000 controls. Click on the thumbnail, or on the underlined text, to see the larger version (43 KB).
Same classification as Dräger AV-E except it is minute-volume preset (unique among anesthesia ventilators). VT cannot be set directly, it is calculated from settings of VE and respiratory rate (VE = RR x VT). Inspiratory flow stops when set VT worth of driving gas has been delivered to the driving circuit side of the bellows chamber or if pressure greater than 65 cm water is attained. Thus, a patient requiring peak inspiratory pressure > 65 cm water cannot be mechanically ventilated with this ventilator.
 Ohmeda 7800 controls. Click on the thumbnail, or on the underlined text, to see the larger version (34 KB).
Ohmeda 7800 controls. Click on the thumbnail, or on the underlined text, to see the larger version (34 KB).
This ventilator or the older Ohmeda 7900 Smart-VentTM were standard on newer Excel or Modulus machines. Same classification as Dräger AV2 ventilator; VT preset. Tidal volume, respiratory rate, inspiratory flow and pressure limit controls are present.
![]() Ohmeda 7900 controls. Click on the thumbnail, or on the underlined text, to see the larger version (34 KB).
Ohmeda 7900 controls. Click on the thumbnail, or on the underlined text, to see the larger version (34 KB).
Same classification as Dräger AV ventilator, VT preset. Microprocessor control delivers set VT, in spite of changes in fresh gas flow, small leaks, and absorber or bellows compliance losses proximal to the sensors. These flow sensors are placed between corrugated plastic breathing circuit and the absorber head, in both limbs. These are connected to pressure transducers in the ventilator. Compliance losses in the breathing circuit corrugated hoses are not corrected, but these are a relatively small portion of compliance losses.
The first "modern" ventilator- it offered such desirable features as integrated electronic PEEP control, and pressure-controlled ventilation (PCV) mode. It has been reported that the sensors can be quite sensitive to humidity, causing ventilator inaccuracy or outright failure. The problem may be more likely when active airway humidifiers are used (see footnote 10).
Controls are similar to the 7800. Users should be vigilant for cracked tubing in the flow sensors, which are located where the breathing circuit corrugated hoses attach to the absorber head. Leaks here have been reported to cause inability to ventilate, either mechanically or manually. When these failures occur, the ventilator may indicate alarm messages like "VT" or "Apnea", rather than "Check sensor". Flow sensor tubing must be vertical, must be changed regularly, and sensors must be in the proper side (inspiratory or expiratory). Although the sensor plugs are keyed by size and shape, if both sensors come off the absorber head when the circuit is changed they can be inadvertently replaced on the wrong side.