
The Anesthesia Gas Machine 2026
Michael P. Dosch PhD CRNA (ret), Darin Tharp CRNA MS
University of Detroit Mercy - Nurse Anesthesia
This site is https://healthprofessions.udmercy.edu/academics/na/agm/.
Revised Feb. 2026

The Anesthesia Gas Machine 2026
Michael P. Dosch PhD CRNA (ret), Darin Tharp CRNA MS
University of Detroit Mercy - Nurse Anesthesia
This site is https://healthprofessions.udmercy.edu/academics/na/agm/.
Revised Feb. 2026
The hospital medical gas pipeline is the primary gas source for the anesthesia gas machine.
Oxygen is produced by fractional distillation of liquid air. It is stored as a liquid at -150 to -175 degrees C in a large flask (because the liquid occupies 1/860 of the space the gas would occupy). Safety systems and regulators send oxygen to the hospital pipeline at approximately 50 psi; which is therefore the normal working pressure of the anesthesia delivery system.
Nitrous oxide is stored as a liquid, at ambient temperature, in large tanks (745 psi- H tank) connected to a manifold which regulates the pipeline pressure to approximately 50 psi.
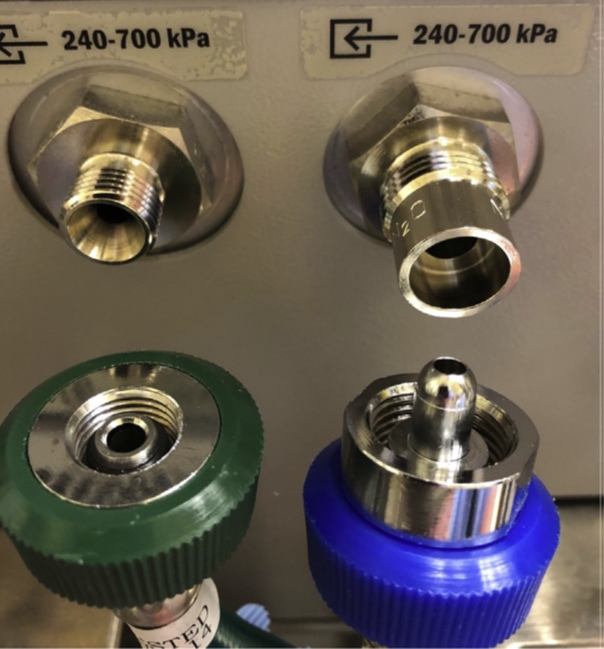
Pipeline inlets (near the yoke blocks for cylinders) are connected with DISS (diameter index safety system) non-interchangeable connections. The check valve, located downstream from the inlet, prevents reverse flow of gases (from machine to pipeline, or to atmosphere), which allows use of the gas machine when pipeline gas sources are unavailable, or when pipeline hoses are disconnected.
|
Diameter index safety system. Click on the link to see the larger version. |
Standards for cylinders are written by the U.S. Department of Transportation (DOT), the Compressed Gas Association, the National Fire Protection Association, and the American Society of Mechanical Engineers. US DOT regulations have the force of law, as do Food and Drug Administration (FDA) regulations on the quality and purity of the medical gas contents.
Capacity, color, markings of cylinders: figures from different sources vary slightly. The table is based on CGA Pamphlet P-2.
|
Gas |
Color |
Service Pressure |
Capacity |
Pin Position |
|
Oxygen |
green (white) |
1,900 |
660 |
2-5 |
|
Nitrous Oxide |
blue (blue) |
745 |
1,590 |
3-5 |
|
Air |
yellow |
1,900 |
625 |
1-5 |
Calculating the time remaining for a cylinder If the pipeline oxygen supply fails, it s an emergency, and the patient only has the contents of the E size oxygen cylinder on the machine to sustain them (before switching to room air and bag-valve-mask as a last resort).
Since the timeline for restoration of pipeline supplies is unpredictable, and the supply of E-sized oxygen cylinders is finite, you must have a means to calculate how long the oxygen cylinder on the machine will last. It s a perennial Board-type question- but it has real clinical importance. Use this equation to solve for minutes your E tank will last.[1].
| Minutes remaining = (0.3 x Gauge pressure psi) ÷ Oxygen Flow L/min |
Example: Your oxygen tank pressure gauge reads 1000 psi. How long can an O2 flow of 2 L/min be maintained? (The tank will last approximately 150 min, at an oxygen flow of 2 L/min).
Cylinder valve - is the most fragile part, so protect it during transport. Consists of
The safety relief device is composed of at least one of these: frangible disc (bursts under extreme pressure), fusible plug (Wood's metal, which has a low melting point), or safety relief valve (opens at extreme pressure).
The hanger yoke:
The check valve in the cylinder yoke functions to:
For more detail, download rules for compressed gases- safe handling or the Compressed gas safety guide.
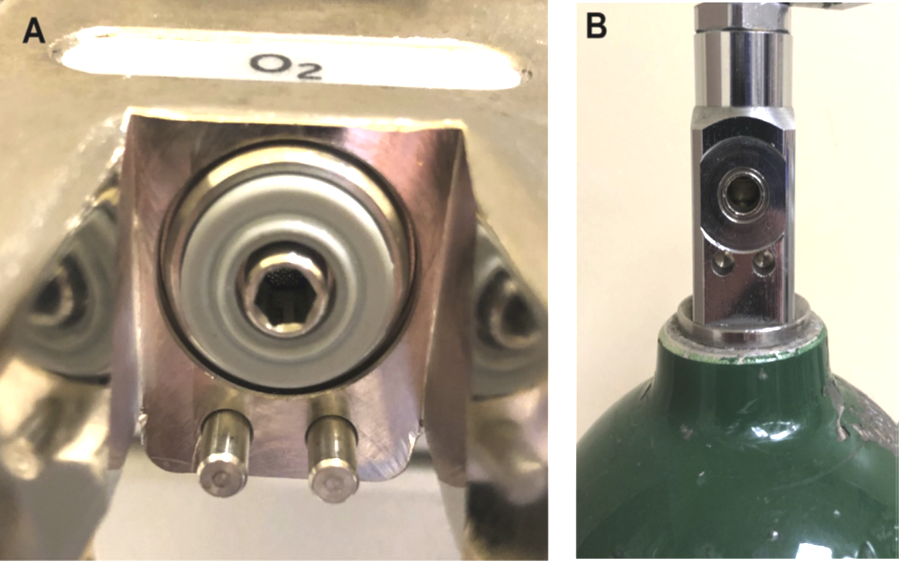
|
Pin-index safety system. Click on the link to see the larger version. |
Main electrical power is supplied to the gas machine through a single power cord which can become dislodged. Because of this possibility, as well as the possibility of main electrical power loss, new gas machines must be equipped with battery backup sufficient for at least 30 minutes of limited operation. What functions remain powered during this period is device-specific, so one must familiarize oneself with the characteristics of each model.
Convenience receptacles are usually found on the back of the machine so that monitors or other equipment can be plugged in. These convenience receptacles are protected by circuit breakers or fuses. In theory, blowing a fuse in one of these circuits should not affect the operation of the rest of the machine. However, loss of monitors is a risk. In view of the easy availability of electrical receptacles in the OR, one should never allow any electrical devices to be plugged into the back of the anesthesia machine.[2].
One should avoid plugging devices into these convenience receptacles which turn electrical power into heat (e.g. air or water warming blankets, intravenous fluid warmers, fiberoptic light sources) for several reasons. First, these devices draw a lot of amperage (relative to other electrical devices), so they are more likely to cause a circuit breaker to open. Second, the circuit breakers on the machine are in non-standard locations (so check for their location before your first case). If a circuit breaker opens, all devices on that circuit will stop functioning. If you are not familiar with the circuit breaker location, valuable time may be lost while a search is conducted. Finally, in some workstations, the circuits are protected by fuses. If a fuse blows it cannot be reset, and the machine must be taken out of service until a replacement fuse can be installed.
Devices (or techniques) which do not rely on wall outlet electrical power include:
Devices which require wall outlet electrical power include:
Generally, hospitals have emergency generators that will supply operating room electrical outlets in the event power is lost. But these backup generators are not completely reliable. Troianos reports on a 90 minute interruption in power during cardiopulmonary bypass, complicated by almost immediate failure of the hospital generators.[3]. One unanticipated hazard was injuries to personnel as they went to fetch lights and equipment through dark hallways.
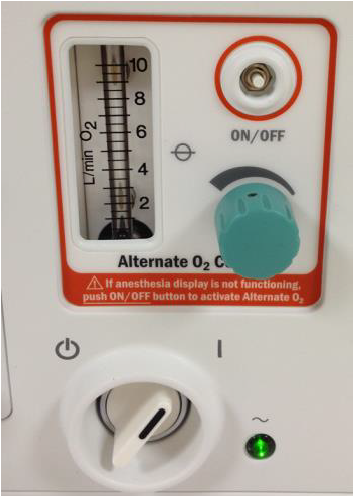
In electrical failure, loss of room illumination, mechanical ventilation and physiologic monitors are the principal problems. In general, current gas machines have battery backup sufficient for 30 minutes of operation (or more)- but perhaps (depending on the model) without patient monitors or mechanical ventilation. For example, GE Aisys provides gas and vapor delivery and all monitors (oxygen, volume and pressure, gas monitoring) for at least 30 minutes if main electrical power is lost. New electronic gas mixers (e.g. Aisys, Perseus) require a backup pneumatic/mechanical flowmeter ("Alternate/ Emergency O2" flow control).
|
Alternate (Emergency) O2 on Aisys. Click on the link to see the larger version. |
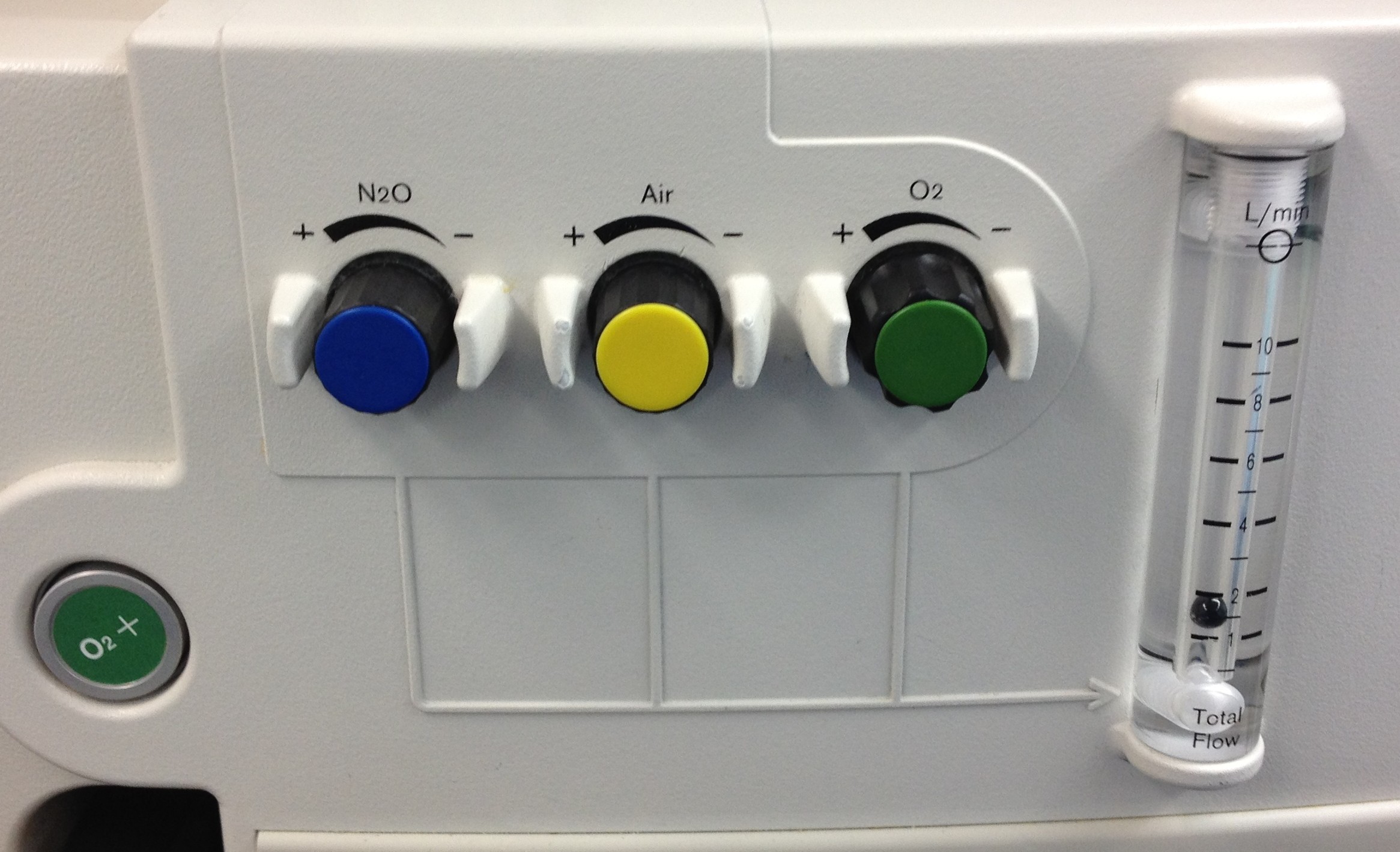
Glass-tube flowmeters with digital display of flows often have a backup common gas outlet flow meter which indicates total fresh gas flow (Fabius GS, Apollo).
|
Apollo- Flowmeter controls & common flowmeter. Click on the link to see the larger version. |
New gas machines which retain pneumatic-mechanical (knob needle valve & glass tube) flowmeters and traditional variable bypass vaporizers (e.g. Aespire, Aestiva, Mindray A1) have an advantage in that delivery of gases and agent can continue indefinitely- but how long do you want to continue surgery by flashlight, with anesthesia monitored by the five senses?
It remains critical to understand and anticipate how each anesthesia workstation functions (what parts and for how long) when main electrical power is lost. The best place to find this information is in the operator's manual. Also see the excellent article, How do I prepare for OR power failure? from the APSF Newsletter (2016).[4].
Pipeline sources are not trouble free: contamination (particles, bacteria, viral, moisture), inadequate pressure, excessive pressures, and accidental crossover (switch between oxygen and some other gas such as nitrous oxide or nitrogen) are all reported. These are not theoretical problems. Intraoperative hypoxemia related to pipeline gas contamination continues to be reported in the US, as recently as 2024, involving the death of an 8-year old after a three-minute biopsy.[5]. Anesthetists' responses to oxygen pipeline failure (and crossover) were inadequate when these events were studied via simulation. [6].
For a crossover, one must
Crossover means a switch in gas supply lines, such that there is a non-oxygen gas (e.g. nitrous oxide or nitrogen) flowing from the oxygen pipeline. The principal sign of crossover is a declining FIO2 in spite of apparently adequate oxygen flow. You must disconnect the pipeline supply, since gas will flow from whichever source is at a higher pressure- the contaminated pipeline (at 50 psi) or the emergency tank supply of oxygen (supplied to the machine at 45 psi).
If oxygen pipeline pressure is lost entirely, the principal signs are a low oxygen pipeline pressure alarm, and activation of the fail safe system. Similar to a crossover, first you must open the backup oxygen cylinder fully. Anesthetists are not in the habit of doing this. We need to open the cylinder only partially to check it, but must open it fully when we are using it (else it may not empty completely). Second, although it is not strictly necessary, I advocate disconnecting the pipeline supply if pipeline pressure is lost for two reasons:
It is recommended to ventilate manually when pipeline oxygen is unavailable in machines which use oxygen in whole or part as the driving gas (gas that compresses the ventilator bellows). Using mechanical ventilation in a bellows-type ventilator in the absence of pipeline oxygen can use an entire E cylinder of oxygen (approximately 600 L) in an hour or less.[8]. This admonition to ventilate manually if pipeline oxygen supply pressure is lost) applies to many but not all gas machines. The exceptions are piston ventilators, which do not use driving gas or bellows at all (Fabius GS, Apollo), or turbine ventilators (Perseus). They only require electrical power for the ventilator. A second exception may be the Aisys, which can sense the loss of oxygen and switch to piped air as the driving gas (if it is available), which would also tend to preserve the cylinder oxygen for the fresh gas flow.
It is better to manually ventilate with the breathing circuit on the machine if you can (not with a bag-valve-mask). Using the breathing circuit allows you to administer volatile agent.
[1] See Oxygen Tank Duration Calculator at https://www.omnicalculator.com/other/oxygen-tank-duration. They use a conversion factor of 0.28 (various sources give different values for E tank contents when full; they use 680 L), but 0.3 is relatively easy to remember and accurate enough for the purpose.
[2] Anaesthesia 2002 Nov;57(11):1134-5. doi: 10.1046/j.1365-2044.2002.28741.x
[3] Troianos CA. Complete electrical failure during cardiopulmonary bypass. Anesthesiology. 1995 Jan;82(1):298-302. doi: 10.1097/00000542-199501000-00037.
[4] Holland EL, Hoaglan CD, Carlstead MA Beecher RP, Porteus GH. How Do I Prepare for OR Power Failure? APSF Newsletter 2016 Feb;30(3) at https://www.apsf.org/article/how-do-i-prepare-for-or-power-failure/ Accesssed Feb 5, 2026
[5] AHRQ 2024 at https://psnet.ahrq.gov/web-mm/hypoxic-gas-supply-cross-connected-pipelines Accessed Feb 5, 2026;
Bernstein DB, Rosenberg AD. Intraoperative Hypoxia from Nitrogen Tanks with Oxygen Fittings. Anesth Analg 1997 Jan; 84(1):225-227;
Elizaga AM, Frerichs RL. Nitrogen Purging of Oxygen Pipelines: An Unusual Cause of Intraoperative Hypoxia. Anesth Analg 2000 July; 91(1):242-243 DOI: 10.1213/00000539-200007000-00045.
[6] Anaesthesia 2007;62(2):122 doi 10.1111/j.1365-2044.2006.04899.x;
Anesth Analg 2010 May;110(5):1292-1296.DOI: 10.1213/ANE.0b013e3181d7e097;
Anesth Analg 2006 Mar;102(3):865-867. DOI: 10.1213/01.ane.0000195548.38669.6c
[7] Anaesthesia 2007;62(2):122 doi 10.1111/j.1365-2044.2006.04899.x;
Anesth Analg 2010 May;110(5):1292-1296.DOI: 10.1213/ANE.0b013e3181d7e097;
Anesth Analg 2006 Mar;102(3):865-867. DOI: 10.1213/01.ane.0000195548.38669.6c;
Weller et al. Anesthetists management of oxygen pipeline failure: Room for improvement. Anaesthesia 2007;62:122 doi 10.1111/j.1365-2044.2006.04899.x;
University of Florida Department of Anesthesiology. Proposed hypoxic O2 pipeline algorithm. 2002 at https://vam.anest.ufl.edu/Hypoxicalgorithm.pdf Accessed Feb 5, 2026.
[8] Anesth Analg 2002 Jul;95(1):148-50. doi: 10.1097/00000539-200207000-00026.